- Approximately 16.7% of live births in 2021 were affected by hyperglycemia during pregnancy, with the vast majority due to gestational diabetes.
- Around 10–14% of pregnancies in India are impacted by gestational diabetes, with even higher prevalence in urban areas.
“Gestational diabetes was once rare. Today, I see more women struggling with it during pregnancy. This rise isn’t due to one single factor—it’s the result of evolving lifestyles, later pregnancies, and increasing obesity. Understanding the root cause is vital for prevention and early management.”So, what exactly is gestational diabetes—and why is it showing up more than ever before?
Let’s start by understanding what’s actually happening inside the body when gestational diabetes strikes.
What Is Gestational Diabetes?
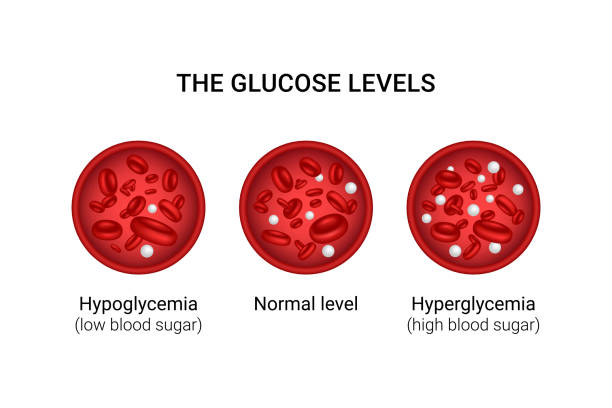
Gestational diabetes mellitus (GDM) is a condition characterized by elevated blood glucose levels that first appear during pregnancy. It typically develops in the second or third trimester and usually resolves after delivery—but its effects can linger if not properly managed.
Here’s what happens: during pregnancy, the placenta produces hormones that can interfere with the mother’s insulin— the hormone responsible for controlling blood sugar. In some women, this leads to insulin resistance, where the body no longer uses insulin effectively, causing blood sugar levels to spike.
Although temporary, GDM significantly increases the risk of complications for both the mother and the baby, making early detection and management essential.
Causes of Gestational Diabetes
The surge in GDM cases isn’t accidental—it’s tied to a mix of lifestyle changes, biological trends, and environmental factors that have evolved over the past few decades.
Here are key contributors to the rise:
Increased Maternal Age
Many women today choose to have children later in life due to career goals, financial planning, or personal preferences. Unfortunately, age increases insulin resistance, making older expectant mothers more susceptible to GDM.
Rising Obesity Rates
Sedentary lifestyles and high-calorie diets are becoming the norm globally. In India, urban women are particularly at risk due to decreased physical activity and unhealthy eating habits. Excess body fat significantly impairs insulin function.
Urbanization and Processed Diets
Heavily processed foods rich in sugars and fats are replacing traditional whole foods. Coupled with stress and minimal physical exertion, this dietary shift is contributing to impaired glucose tolerance.
Increased Use of Fertility Treatments
Assisted reproductive technologies (ART) can slightly elevate the risk of GDM, especially in women already prone to insulin resistance.
Ethnic and Genetic Predisposition
South Asian women, including Indian women, have a higher genetic susceptibility to insulin resistance and gestational diabetes, making ethnicity a significant factor.
Dr. Himali Maniar, a respected fertility-focused gynecologist in Bopal, adds,
“What we see today is a culmination of modern choices colliding with biological limitations. Managing weight, planning timely pregnancies, and routine screenings can make a big difference in preventing GDM.”
Risk Factors You Should Know
- If you had gestational diabetes before, there’s a higher chance it will recur.
- A parent or sibling with type 2 diabetes increases your risk.
- Women with a BMI over 25 are more likely to develop insulin resistance.
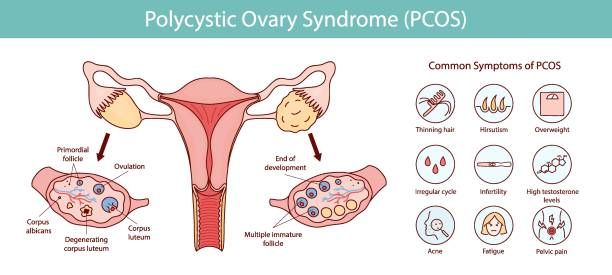
- Polycystic Ovary Syndrome (PCOS) is linked with insulin issues.
- Twin or triplet pregnancies can increase metabolic strain on the body.
- A previous delivery of a baby weighing more than 4kg could signal undiagnosed GDM.
“If you fall into any of these categories, early glucose screening should be a priority. It’s not just about preventing diabetes—it’s about safeguarding long-term health for you and your child.”
Signs & Symptoms of Gestational Diabetes
Gestational diabetes can be subtle, often going unnoticed without proper screening. However, some women may experience the following symptoms:
- Unusual Thirst
- Frequent Urination
- Fatigue
- Blurred Vision
- Frequent Urinary or Vaginal Infections
However, many women show no outward symptoms, which is why glucose testing between weeks 24 and 28 is standard practice.
Health Risks of Untreated Gestational Diabetes
Unchecked gestational diabetes can lead to significant complications for both mother and baby. Here’s how it can affect health outcomes:
For the Baby:
- Excessive birth weight (macrosomia)
- Premature delivery
- Breathing difficulties
- Increased risk of childhood obesity and type 2 diabetes
For the Mother:
- Higher chance of cesarean delivery
- Risk of preeclampsia (high blood pressure during pregnancy)
- Long-term risk of developing type 2 diabetes
Dr. Himali Maniar, a compassionate gynecologist in Bopal, emphasizes,
“What many don’t realize is that unmanaged GDM isn’t a short-term issue—it sets the stage for long-term health challenges for both mother and child. Timely diagnosis and lifestyle interventions can alter this trajectory.”
How Gestational Diabetes Is Managed Today

Modern management of gestational diabetes focuses on monitoring, lifestyle changes, and, when necessary, medications. Here’s what a standard approach includes:
- Expecting mothers are advised to check their glucose levels multiple times a day to maintain targets.
- A personalized, nutrient-rich diet emphasizing complex carbs, lean proteins, and fiber can help stabilize blood sugar.
- Walking, prenatal yoga, and light aerobic activity improve insulin sensitivity.
- If lifestyle changes aren’t sufficient, doctors may prescribe insulin or oral hypoglycemics.
- Regular fetal ultrasounds and non-stress tests help ensure the baby’s well-being.
Dr. Himali Maniar, a results-driven obstetrician in Bopal, says:
“The beauty of modern GDM care is personalization. With collaborative planning, we empower women to take control of their pregnancy and emerge stronger.”
FAQs on GDM
Can a healthy person get gestational diabetes?
Yes. Even women who are otherwise healthy and active can develop GDM due to hormonal shifts during pregnancy. It’s not solely tied to weight or diet—age, genetics, and even stress levels play a role.
Does GDM affect the baby’s long-term health?
It can. Babies born to mothers with GDM are at higher risk of obesity, type 2 diabetes, and metabolic issues later in life. However, proper prenatal care can significantly reduce these risks.
What’s the ideal diet for gestational diabetes?
A balanced diet rich in whole grains, vegetables, lean proteins, and healthy fats.
Foods with a low glycemic index should be prioritized.
Frequent small meals help avoid glucose spikes.
How soon should I start physiotherapy for PGP?
As early as possible. Starting physiotherapy at the onset of symptoms often prevents worsening and supports better mobility throughout pregnancy.
Can exercise reduce the risk of developing GDM?
Absolutely! Physical activity boosts insulin function and helps maintain a healthy weight—two major factors in GDM prevention.
References:
https://www.mayoclinic.org/diseases-conditions/gestational-diabetes/symptoms-causes/syc-20355339
https://diabetes.org/living-with-diabetes/pregnancy/gestational-diabetes
Disclaimer: The information shared in this content is for educational purposes only and not for promotional use.